The health and wellbeing of our future lies with adolescents
The below post has been written by Georgia Lockwood Estrin, who is not only a Research Fellow for Mental Health Innovation Network (MHIN), but a passionate advocate for youth mental health and wellbeing. Georgia, was also a panellist at our London launch on May 10.
The Commission is delighted to see our messages being translated and disseminated by various organisations from around the world. Our media page includes links to articles talking about our work and our report.
Adolescence is a critical time in an individual’s development, and it lays the foundations for health and wellbeing in adulthood. Characterised by dynamic brain changes, during adolescence the brain’s reward system is remodelled and connectivity substantially increases between different brain networks — these processes are affected by social and nutritional environments, as well as by negative exposures such as substance use. This shapes the capabilities and behavioural patterns (including health behaviours) that an individual takes forward into adult life.
Despite this, adolescence is a long neglected age group, especially in terms of health care. Adolescents often fall through the gap between paediatric and adult health services, and have until recently been overlooked in the larger picture of global health and social policies. Health promotion in this age group also presents challenges because adolescents have reduced health-seeking practices compared to adults, and there is a paucity of research to provide insight into the needs of this age group. Compounding these challenges, as a society we are undergoing great changes, with global trends increasingly promoting unhealthy lifestyles, coupled by high rates of global unemployment, reduced family stability and mass migration. These changes especially affect this age group, making them even more vulnerable to adverse physical and mental health outcomes. Adolescents need services specialised specifically for their needs in our fast-paced changing social environment.
In response to these needs, and current shifts in determinants of health, The Lancet partnered with The University of Melbourne, University College London, the London School for Hygiene and Tropical Medicine and Columbia University in order to establish a Commission on Adolescent Health and Wellbeing, which was launched earlier this month on 10th May 2016.
Lancet Commission on adolescent health and wellbeing
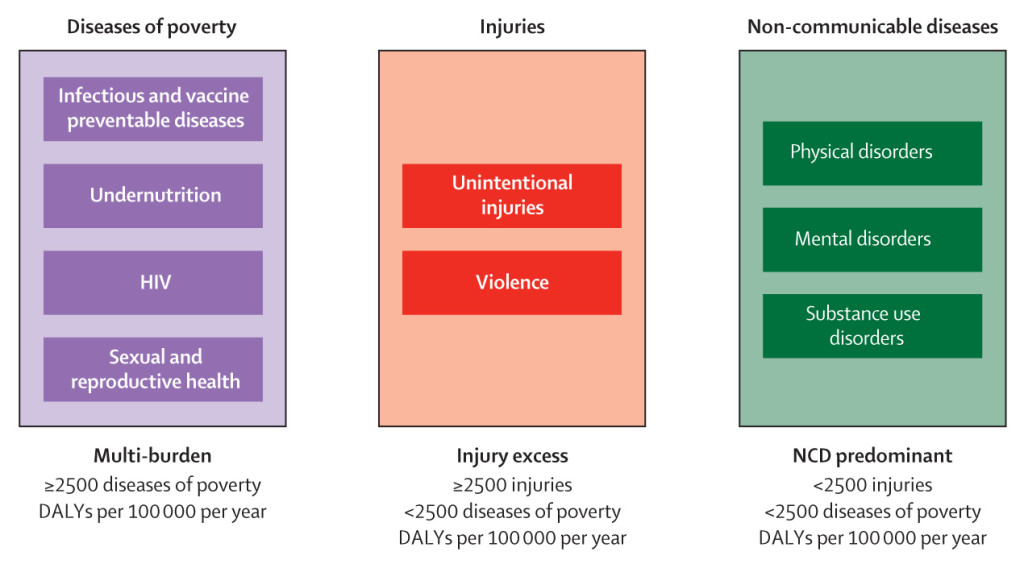 Figure: Country categorisation based on adolescent burden of disease. Categorisation of countries into three groups according to adolescent burden of disease and reflecting passage through epidemiological transition. DALYs: disability-adjusted life-years. NCD: non-communicable diseases.1
Figure: Country categorisation based on adolescent burden of disease. Categorisation of countries into three groups according to adolescent burden of disease and reflecting passage through epidemiological transition. DALYs: disability-adjusted life-years. NCD: non-communicable diseases.1 A fundamental finding from the commission was the substantial reduction in the disease burden from infectious diseases and sexual and reproductive health seen over the last 20 years – this was found in every country profile. A smaller, but still impressive, improvement has been made for injury and violence related disease burden in each country profile. In stark contrast however, there has been almost no change in the disease burden of chronic physical and mental disorders in any country profile between the 1990’s and today – an eye-opening result. This reveals the urgent need to invest in research and services for adolescent mental health and preventative interventions for chronic illness, in order to make headway in improving these outcomes.
“There has been almost no change in the burden of disease for chronic physical and mental disorders in any country profile between the 1990’s and today.”
In light of these findings, the commission discusses enabling factors as well as challenges faced by adolescents relating to their health risks, including demographic transitions, protective systems, family function, education, technology and legal frameworks. The highlights from the commission, specifically those relating to mental health, and recommendations for investment and research to improve outcomes will be further discussed below.
Adolescent mental health
Mental health problems affect 10-20% of children and adolescents worldwide and account for a large portion of the global burden of disease.2 They also commonly emerge during adolescence, with many persisting into adulthood — in fact studies in adults show that most mental disorders begin before the age of 25, and most often present for the first time between 11-18 years. Adolescence is therefore a critical window of opportunity to prevent the emergence and progression of mental disorders, which could decrease the disease burden throughout the life course.

However, major challenges exist for early intervention, including large detection and treatment gaps – i.e. the difference between the number of people needing diagnosis and treatment, and the number who are actually receiving it. This is particularly the case in low and middle income countries (LMIC), where there is little awareness about these disorders, as well as a scarcity of mental health professionals to provide much needed interventions. These barriers need to be overcome before we can significantly improve mental health outcomes. In order to narrow these gaps, a public health approach to detection and treatment is required, such as utilisation of non-specialised frontline health workers in routine health care settings and community platforms – a strategy to overcome human resource shortages in LMIC, which has gained substantial evidence for improving mental health outcomes.3
Family environment
One of the key risk factors of adverse mental health outcomes in adolescents discussed in the commission was that of family environment and instability. Families provide the main protective and enabling setting for the health and wellbeing of children and adolescents. Despite this, there is a striking knowledge and research gap on the effect of family influences on adolescent health. Adolescents living in families with difficulties are at greater risk of suicide, depression, eating disorders, and substance abuse.4 Family violence specifically has profound effects, with exposure to violence being associated with substance abuse, but also with education failure and a continuation of a negative cycle of engagement in their own abusive relationships.5
Parenting capacity, especially those around monitoring and supervising adolescent activities, are important factors in determining health risks and modifying unhealthy behaviours. In fact, better parent-adolescent communication is associated with better social functioning and fewer mental health problems.6 Therefore, preventative interventions aimed at improving parent-adolescent communication may have huge advantages by enabling protective environments and improving both physical and mental health outcomes.
Education: schools and technology
A key recommendation from the commission was that of investing in secondary school education. Education itself is an important determinant of health as well as a powerful influence on socioeconomic progress; the benefits are particularly true for women in high-income countries for both physical and mental health.7 Unfortunately, there has been little research on the benefits of education for adolescents in LMIC.
The commission, however, made great headway in improving our understanding of the health effects of education in this demographic, finding strong associations between the average number of years in education and adolescent birth rates, maternal mortality, and injury mortality. This was demonstrated using UN sourced data on the average number of years in education for young men and women aged between 15-24 years in 187 countries, and between 1970-2015. One study of a cohort in the Philippines established that adolescents with secondary education had a lower rate of health problems by more than 50% compared to those with primary education alone, and this was specifically true for mental health, alcohol use and sexual health. These results led to one of the key recommendations of the commission – making increased investments in education would bring improvements in health, and especially marked reductions in total adolescent birth rates for girls and young women.
“Adolescents with secondary education had a lower rate of health problems by more than 50% compared to those with primary education alone.”
It is also important to recognise the unique opportunity provided by schools to implement interventions to improve health outcomes in adolescents; for example the commission found strong evidence for school-based health services that improve sexual and reproductive health. There was also promising, but not yet a strong evidence base, for school-based mental health services – highlighting this as an important research area for investment.
However, whilst the health and wellbeing benefits of expanding secondary education are immense, there are many forces that operate to exclude adolescents from such education. Those individuals not accessing education may be the most marginalised and vulnerable to health problems. For example, adolescents who are without a job or not in any sort of education or training are at increased risk of mental health problems including suicide.8 Therefore interventions aiming to include and empower this vulnerable group must be considered.
“Those individuals not accessing education may be the most marginalised and vulnerable to health problems.”
One crucial and yet under-researched intervention is the use of media and technology, which has the potential to provide a powerful voice for adolescents to actively engage with each other and break barriers of stigma and discrimination. It also has the potential to play a positive role in prevention and promotion of access to clinical services and health education.
The role of technology was explicitly highlighted in the commission, as not only a means to promote health among adolescents, but also to build capacity between different sectors, such as health services, legal services, social services, schools and other, in order to coordinate actions and to improve health outcomes across these dimensions for adolescents worldwide.
Legal frameworks
Whilst technology may provide a key to empowering marginalised adolescents, a significant factor addressed in the commission was the disempowerment of adolescents due to ineffective and inconsistent law and policy. This is a subject often neglected in discussions surrounding adolescent health. High, middle and low income counties all demonstrate inconsistencies in their laws relating to adolescents; for example, the age of criminal responsibility varies from 6 -14 years in US states, and this is compared to the age of majority (the age at which a person is recognised by law as an adult) which is 18-21 years.
“Whilst technology may provide a key to empowering marginalised adolescents, a significant factor addressed in the commission was the disempowerment of adolescents due to ineffective and inconsistent law and policy.”
Loopholes in the law also exist, meaning that policies aiming to protect adolescents and children are not effectively upheld. For example the Child Marriage Act setting the legal age of marriage in India at 18 years is subject to many customary and religious loopholes, leading to the high rate of 47% of women in India being married before they reach 18 years of age. This has many adverse health and emotional outcomes, as girls marrying before 18 years report physical violence twice as often and sexual violence three times as often as those marrying later in life.
Legal frameworks are needed to protect adolescents, but it is not until these inconsistencies and loopholes are addressed that systems can actively provide the support and empowerment needed by this age group.
What are the take-home messages of the commission?
This commission brings to the foreground the challenges as well as opportunities for improving adolescent physical and mental health. The importance of using a multi-sectoral response for improving health outcomes in this age group was explicitly highlighted and is key to moving forward in this field. Other recommendations focused on empowerment and education of this age group, and the UN Secretary-General’s Global Strategy for Women’s, Children’s and Adolescent’s, launched in September 2015, presents an opportunity for much needed investment in this area. However, the scarcity of research into effective interventions for mental health, and the critical need to make progress to improve mental health outcomes in adolescents was a much-needed wake-up call for us all. We need to work together to improve the health of this age group, which has the potential to have lasting effects on their later life and the life of generations to come.
- George C Patton, Susan M Sawyer, John S Santelli, David A Ross, Rima Afifi, Nicholas B Allen, Monika Arora, Peter Azzopardi, Wendy Baldwin, Christopher Bonell, Ritsuko Kakuma, Elissa Kennedy, Jaqueline Mahon, Terry McGovern, Ali H Mokdad, Vikram Patel, Suzanne Petroni, Nicola Reavley, Kikelomo Taiwo, Jane Waldfogel, Dakshitha Wickremarathne, Carmen Barroso, Zulfiqar Bhutta, Adesegun O Fatusi, Amitabh Mattoo, Judith Diers, Jing Fang, Jane Ferguson, Frederick Ssewamala, Russell M Viner. Our future: a Lancet commission on adolescent health and wellbeing. The Lancet, Published Online May 9, 2016. http://dx.doi.org/10.1016/ S0140-6736(16)00579-1
- Kieling C, Baker-Henningham H, Belfer M, et al. Child and adolescent mental health worldwide: evidence for action. Lancet 2011; 378(9801): 1515-25.
- Kakuma R, Minas H, van Ginneken N, et al. Human resources for mental health care: current situation and strategies for action. Lancet 2011; 378(9803): 1654-63.
- Pilgrim NA, Blum RW. Adolescent mental and physical health in the English-speaking Caribbean. Revista panamericana de salud publica = Pan American journal of public health 2012; 32(1): 62-9.
- Volpe JS. Effects of domestic violence on children and adolescents: an overview. 1996. http://www.aaets.org/article8.htm (accessed May 30, 2016).
- McPherson KE, Kerr S, McGee E, et al. The association between social capital and mental health and behavioural problems in children and adolescents: an integrative systematic review. BMC psychology 2014; 2(1): 7.
- Miyamoto K, Chevalier A. Education and health. In: OECD, ed. Improving health and social cohesion through education. Paris: Organisation for Economic Co-operation and Development, 2010: 111–79.
- Benjet C, Hernández-Montoya D, Borges G, Méndez E, Medina-Mora ME, Aguilar-Gaxiola S. Youth who neither study nor work: mental health, education and employment. Salud Publica Mex 2012; 54: 410–17.
By: Georgia Lockwood Estrin, a Research Fellow for Mental Health Innovation Network (MHIN) and affiliated with the Centre for Global Mental Health (CGMH) and London School of Hygiene and Tropical Medicine.
This blog was originally published online at MHIN, view the original here.