News

Perspectives on Data Re-Use
Meeting Children Where They Are: Perspectives on Data Re-Use from the Youth Solutions Labs

Advancing Adolescent Health in the Asia Pacific
Starting 2024 – a new seminar series “Advancing Adolescent Health in the Asia Pacific: A virtual community to share knowledge and support collaboration.”

Adolescent nutrition
This work highlights the effect of nutrition on adolescent growth and development, the role the food environment has on food choices, and which strategies and interventions might lead to healthy adolescent nutrition and growth.

Calling for applications!
Calling all 18-30-year-olds! The Second Commission on Adolescent Health and Wellbeing is looking for five experts to serve on the multi-disciplinary youth review board!

Nairobi meeting
The African Population and Health Research Center recently hosted a meeting of the Second Lancet Commission on Adolescent Health and Wellbeing in Nairobi, Kenya, from May 9 to 11, 2023.

Apply to join the Youth Solutions Labs
Are you between the ages of 16 and 20? Would you like to make a difference in your community? Apply now to help set the global adolescent health and wellbeing agenda for 2024!

WHO Youth Council
Youth Commissioners, Dr. David Imbago-Jácome and Surabhi Dogra join the WHO Youth Council.
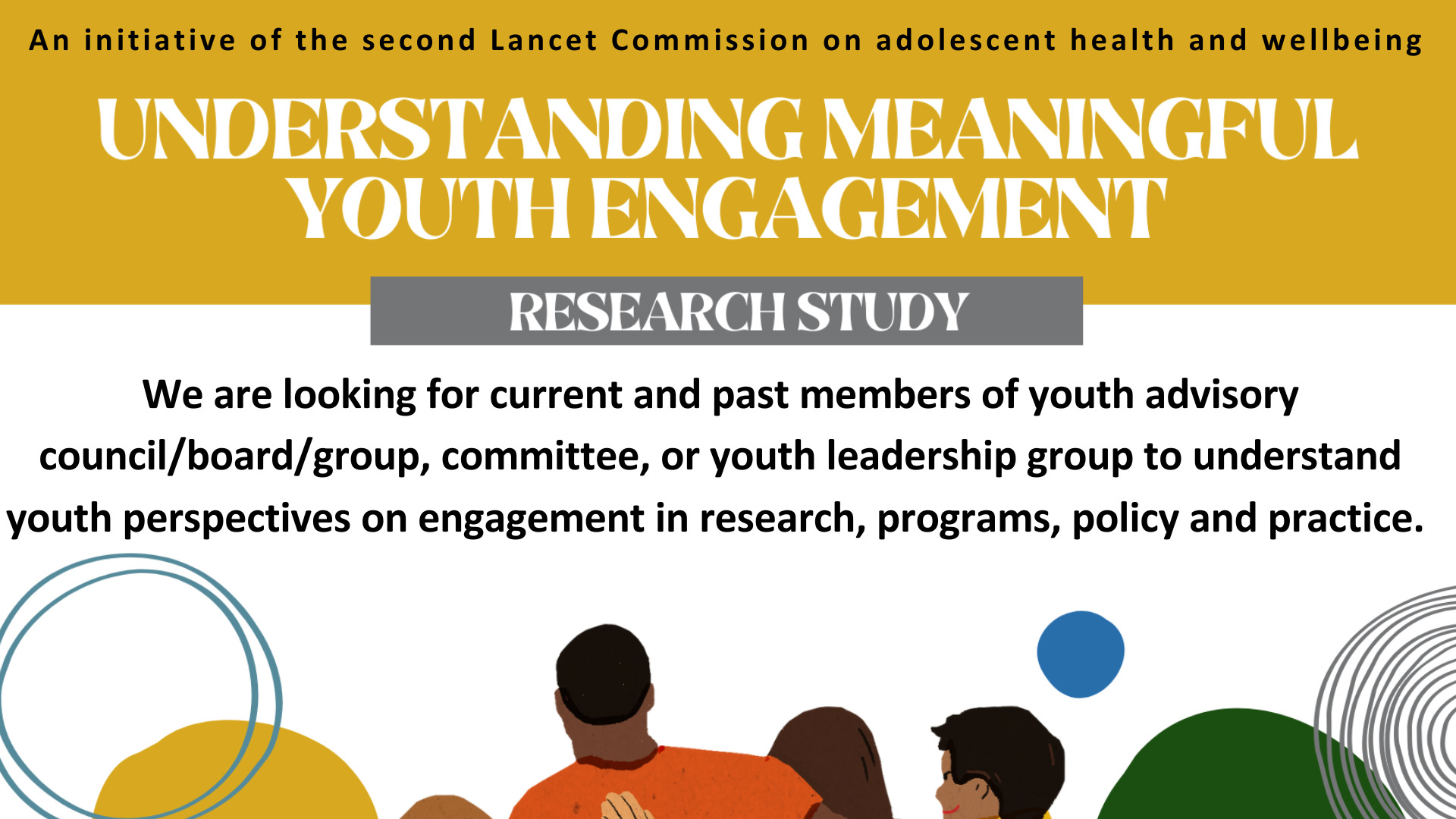
Understanding meaningful youth engagement
We are looking for current and past members of youth advisory councils/ boards/ groups, committees, or youth leadership groups to understand youth perspectives on engagement in research, programs, policy and practice.

What is the evidence to prevent injury among adolescents?
Injury is a leading cause of death and disability among adolescents, yet investment in these preventable harms lag behind that of other issues and investments made in younger children.

Vale Professor George C Patton
It is with great sadness that we advise that Professor George Patton passed away on the 7th December 2022.

Congratulations Prof Degenhardt
Congratulations Professor Louisa Degenhardt on making the top 100 in the list of the world’s best female scientists.

A second Lancet Commission on Adolescent Health and Wellbeing
This Second Lancet Commission on Adolescent Health and Wellbeing seeks to ensure that today’s adolescents have the means to address the unique challenges of their generation.